Past Programs
Since its founding in 1998, the de Beaumont Foundation has invested in programs that improve health through system change and evidence-based solutions. Following are a few of our past programs that reflect our strategic priorities.
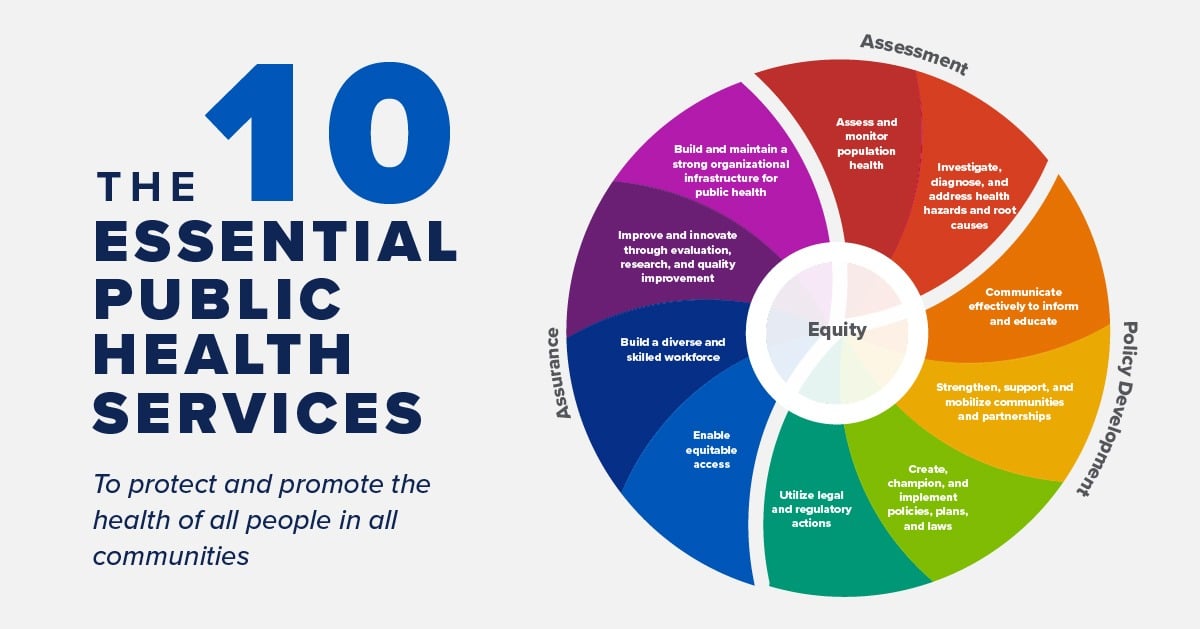
10 Essential Public Health Services
A framework for public health to protect and promote the health of all people in all communities.

Cost-Effectiveness in Public Health
Grantee: Johns Hopkins University Bloomberg School of Public Health

Obesity Data Challenge
The de Beaumont Foundation supported two Obesity Data Challenges that identified effective

Valuing Prevention
The de Beaumont Foundation joined with several other funders to support the creation of an Institute of Medicine (IOM) committee to determine how best to measure the value of community-based

Medicaid and Population Health
Maximizing Public Health Partnerships with Medicaid to Improve Population Health
Upstream Health Priorities for Governors
Tools for state leaders and advocates to promote policies that improve lives

Training for State Health Leaders
Preparing state officials to lead their agencies and improve health for all