Bold Solutions for Healthier Communities

Practicing Disability Inclusion in Health Agencies
One in 4 US adults lives with a disability.1 People with disabilities are present in every community. This means every […]
Talking With Nancy Krieger: Deconstructing Data for Health Equity
The de Beaumont Foundation’s Speaker Series highlights leaders in public health practice, advocacy, policymaking, and other related fields. In her […]

Six Practical Uses of PH WINS for Health Departments
The workforce spoke through the Public Health Workforce Interest and Needs Survey (PH WINS). If your agency hasn’t taken action […]
Partnering with Business at the IMPACT in Public Health Convening
Business and public health both have much to gain when they work together to champion health equity in their communities. […]

Public Health Workforce Challenges Through the Eyes of a Public Health Educator
One in six. One in six respondents to the 2021 Public Health Workforce Interests and Needs Survey (PH WINS) agreed […]

Advice for 2023 Grads: Think Big. Think Policy.
Big thinking. Policy solutions. Unlikely partnerships. These were among the themes our president and CEO, Brian C. Castrucci, DrPH, shared […]

New Actor Map Surveys Landscape of Organizations Supporting Public Health Workforce
The National Consortium for Public Health Workforce Development has launched the Public Health Workforce National Actor Map, an interactive tool […]

From Clinical Care to Population Health: Q&A with 40 Under 40 Honoree Sameer Vohra
Blending his expertise in public health and medicine, Sameer Vohra MD, JD, MA, brings a unique perspective to his role […]

Adults’ Mental Health in the COVID Context
May is Mental Health Awareness Month, a moment to recognize and elevate the need for more research, education, and awareness […]
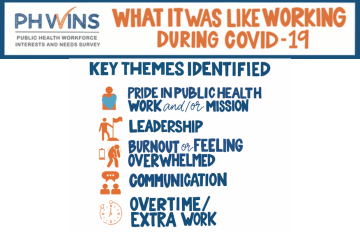
It’s More than Burnout: Moral Injury in the Public Health Workforce
In 2021, one in four public health workers was considering leaving their organization in the next year; 44% were considering […]

On Relationship Building and the Power of Partnerships: Q&A with 40 Under 40 Honoree Sami Jarrah
From working in academia to local government and back to academia, 40 Under 40 in Public Health honoree Sami Jarrah, […]

Gifts for Your Favorite Public Health Graduate
This spring, many new public health practitioners will be graduating from their programs, joining our ranks in improving public health […]
