Bold Solutions for Healthier Communities

40 Under 40 Spotlight: Joseph Kanter
Read Joseph’s bio. See all 40 Under 40 honorees. Five Questions for Joseph 1. Who or what inspired you to […]
Media Coverage of COVID-19 Highlights Local Leadership and Constraints
The response to the COVID-19 outbreak has shown public health at its best, with state and local agencies taking all […]
‘While We Are Waiting, People Are Getting Sick’: Dr. Brian Castrucci on the Coronavirus Response
When a pandemic is looming, “it’s not the time to have the conversation” about funding health departments, said Brian Castrucci, […]

40 Under 40 Spotlight: Jeffrey Hom
Read Jeffrey’s bio. See all 40 Under 40 honorees. Five Questions for Jeffrey 1. Who or what inspired you to […]
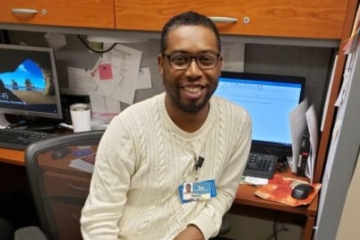
40 Under 40 Spotlight: Devin Hursey
Read Devin’s bio. See all 40 Under 40 honorees. Five Questions for Devin 1. What is one of the most […]

Community Approaches to Systems Change
Why is it that improving community health is so challenging? One answer is that because doing so requires change that […]

40 Under 40 Spotlight: Brett Harris
Read Brett’s bio. See all 40 Under 40 honorees. Five Questions for Brett 1. Who or what inspired you to […]

40 Under 40 Spotlight: Jessica Gehle
Read Jessica’s bio. See all 40 Under 40 honorees. Five Questions for Jessica 1. Who or what inspired you to […]

40 Under 40 Spotlight: Alison Traynor
Read Alison’s bio. See all 40 Under 40 honorees. Five Questions for Alison 1. Who or what inspired you to […]
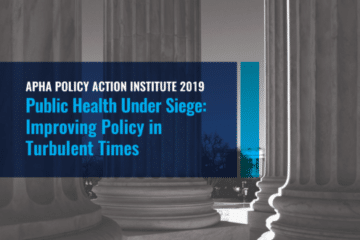
APHA Policy Action Institute 2019: Proceedings
The 2019 American Public Health Association Policy Action Institute was a dynamic event that brought together advocates, leaders at all […]

40 Under 40 Spotlight: Julian Drix
Read Julian’s bio. See all 40 Under 40 honorees. Five Questions for Julian 1. What is one of the most […]

What Does It Take to BUILD Health? Q&A with Emily Yu
The BUILD Health Challenge® (BUILD) welcomed 18 new awardees to its third cohort in November. These communities throughout the […]
