Bold Solutions for Healthier Communities
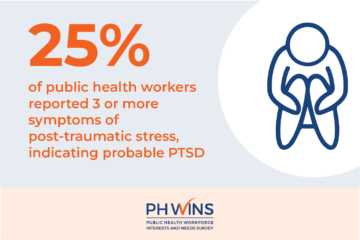
Examining and Addressing Post-Traumatic Stress among Public Health Workers
Government public health workers played an essential role in responding to the COVID-19 pandemic, and their mental health suffered in […]
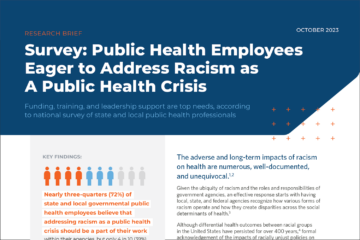
PH WINS Data: Public Health Workers Eager to Address Racism as a Public Health Crisis
The adverse and long-term impacts of racism on health are numerous, well-documented, and unequivocal. The COVID-19 pandemic, the murder of […]

Bolstering Workforce Diversity Matters for the Next Generation of Public Health Professionals
As a Black woman and current Master of Public Health graduate student, I find it imperative to see minorities, especially […]

New Class of 40 Under 40 in Public Health Reflects Resilient and Impactful Workforce
The de Beaumont Foundation today announced its third class of 40 Under 40 in Public Health honorees, recognizing rising leaders who […]

Addressing Inequities in Black Maternal Health Through Community Engagement
Black women’s advocacy has helped to secure crucial rights in American policy, from advancing voting access to dismantling segregation. Regrettably, […]

Navigating Resource-Sharing Agreements: Key Insights for Successful Relationships
Despite operating under constraints such as limited resources and staff, governmental public health departments are committed to serving their communities […]
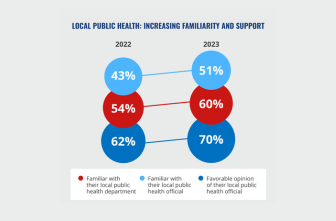
Poll: Americans Strongly Support Health Departments and Services
Americans are more familiar with and supportive of their local health officials than at the start of the COVID-19 pandemic, […]

Four U.S. Communities Receive a $5M Investment to Create Data Ecosystems Centering Health Equity and Racial...
Today, we announced newly awarded grants to communities in Arizona, Maryland, Oregon, and Pennsylvania to pursue data-driven initiatives that advance […]
We Can Do This: New Book Policy Engagement is a Field Guide for Public Health
Shaping systems and policies is critical to improving people’s health; and influencing health outcomes requires understanding the inner workings of […]

Improving Employee Health and Retention Rates in Michigan
The Michigan Health Improvement Alliance, Central Michigan District Health Department, local manufacturer Vantage Plastics, and Vantage’s nonprofit outreach arm The […]

Promoting Health Equity: Five Actions to Consider
For many in public health, the term “equity” has become more of a buzzword than a call to action. Health […]

