Bold Solutions for Healthier Communities
Coping in Times of Crisis: Mental Health Resources
In state and local health departments across the country, workers find themselves in an “all-hands-on-deck” situation in the COVID-19 response. […]
Why Public Health Matters: Share Your COVID-19 Story
For months, public health professionals have been working to stop the spread of COVID-19 and protect communities across the country, […]
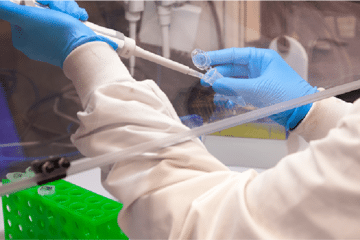
de Beaumont Foundation Makes Contribution to Increase Capacity for COVID-19 Testing
The de Beaumont Foundation today announced a contribution of $100,000 to the Association of Public Health Laboratories (APHL) to support […]

Seeing the Bigger Picture of Public Health Workforce Challenges
With coverage of the coronavirus seemingly everywhere, the role of the public health workforce is front and center in news […]

The COVID-19 Response: 5 Ways Public Health Professionals Can Contribute
As members of the DrPH Coalition, which was launched at the American Public Health Association’s annual meeting in November 2019, […]

Health Leaders on COVID-19: Recognize Inequities, Maintain Connections, Work Together
What does the COVID-19 pandemic reveal about our society’s inequities, and what we can learn from it to ensure a […]

COVID-19 Public Health Resource Roundup
One of our priorities at the de Beaumont Foundation is offering practical solutions to strengthen the public health system and […]

Not All Heroes Wear Capes: COVID-19 Response Inspires T-shirt, Fan Club
Most public health workers are used to working behind the scenes, and that’s fine with them, because their focus is […]

Coronavirus Responders Deserve Better
Republished from Health Affairs (March 19, 2020) with permission from the authors. See the original article on Health Affairs. By […]

Want To Make The Nation More Prepared To Fight Contagious Diseases? Expand Paid Sick Leave
Republished from Health Affairs (March 17, 2020) with permission from the authors. See the original article on Health Affairs. By […]

As Coronavirus Spreads, What Can You Do for Your Community?
It’s hard to comprehend how much life has changed in a month. At the BUILD Health Challenge, we believe the […]

New Report Reveals Differences, Similarities between Public Health and Other State/Local Agencies
Compared with the rest of the government sector, the state and local public health workforce is more diverse, has more […]
