Bold Solutions for Healthier Communities

Stuck at Home? Enroll in an Online Course That Will Build Your Practical Business Skills
Looking for a convenient way to improve your skills in budgeting and financial management from the comfort of your home? […]
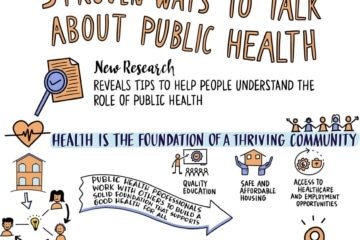
Research Reveals Effective Ways to Talk About Public Health; New Communications Tools Available
Communicating effectively about public health has never been more important, and the de Beaumont Foundation and Aspen Institute have released […]

Use These Three Strategies to Support Staff Entering Leadership Roles
Affordable and safe housing, accessible and safe public transportation, quality education, and many other factors help make our communities healthy. Recent […]

Hollowed-Out Public Health System Faces More Cuts Amid Virus
by Lauren Weber and Laura Ungar and Michelle R. Smith, The Associated Press and Hannah Recht and Anna Maria Barry-Jester […]

Six Takeaways of the KHN-AP Investigation Into the Erosion of Public Health
Local and state public health departments across the country work to ensure that people in their communities have healthy water […]

What Does Racism Have to Do With COVID-19?
Black people and people of color have experienced significantly higher rates of COVID-19 infection and death compared with their white counterparts. It […]

Conflicting COVID Messages Create Cloud Of Confusion Around Public Health And Prevention
By Shefali Luthra, Kaiser Health News Regina Fargis didn’t know what to do. Fargis runs Summit Hills — a health […]

Daring to Lead Boldly: Reflecting on My Time in Public Health Philanthropy
You have to act as if it were possible to radically transform the world. And you have to do it all the time. —Angela Davis […]

CityHealth Names New Co-Executive Directors
Public health and policy leaders Katrina Forrest, JD, and Catherine Patterson, MPP, have been selected to lead CityHealth as co-executive […]
de Beaumont Foundation Partners with Soledad O’Brien to Release ‘Outbreak: The First Response’
“Outbreak: The First Response,” a new documentary tracking the first days and weeks of the COVID-19 pandemic in the United […]

At a Time of Great Need, Public Health Lacks ‘Lobbying Muscle’
By Angela Hart, California Healthline SACRAMENTO — If there were ever a time for more public health funding, health experts […]

Public Health Officials Face Wave Of Threats, Pressure Amid Coronavirus Response
by Lauren Weber and Anna Maria Barry-Jester and Michelle R. Smith, The Associated Press Emily Brown was stretched thin. As […]
