Bold Solutions for Healthier Communities

Poll: 1/3 of Unvaccinated Adults Say FDA Approval of Pfizer Vaccine Will Address Their Safety Concerns
In a national poll conducted just days before the FDA announcement about the Pfizer vaccine, more than one-third of unvaccinated […]

Investing in and Promoting Professional Development
Public health practitioners never stop learning on the job, whether mastering project management, brushing up on policy and law, or […]
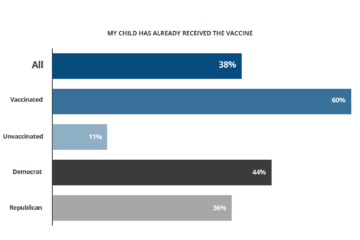
Poll: Confidence in Vaccine Safety Growing; Delta Variant and Pending FDA Approval Could Boost Numbers
With schools beginning to open nationwide, 38% of parents say their child age 12-17 has been vaccinated against COVID-19, according […]

de Beaumont Joins New Coalition to Modernize Public Health System
The de Beaumont Foundation has joined the Bipartisan Policy Center and a coalition of foundations and public health organizations to […]
Your Public Health Workers Are Not Okay
Republished from Substack with the author’s permission. See original, published July 1, 2021. Lack of resources, long (really long) hours, […]

Talking With Michele Okoh: Environmental Justice
The de Beaumont Foundation’s Speaker Series highlights leaders in public health practice, advocacy, policymaking, and other related fields. For Michele […]
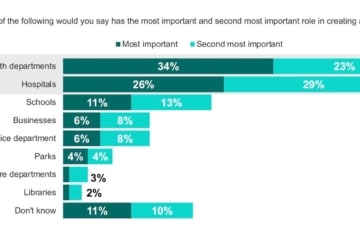
Poll Reveals Strong Support for Public Health Departments and Services
U.S. adults highly value the role of public health departments and the services they provide, according to a new national […]

New Poll: Americans Expect Businesses to Invest in Community Health
As the nation recovers from COVID-19 pandemic, businesses should focus on improving community health, not just employee health, according to […]
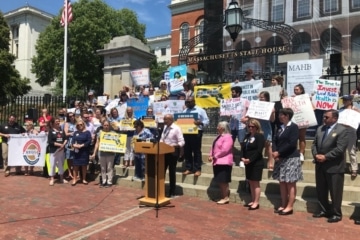
Massachusetts Public Health Supporters Call for Robust, Long-Term Funding
Supporters across the country have been raising their voices to champion sustained investments in public health, especially in the wake […]

Why Public Health Matters to Boise State University Students
Nearly a year since its launch, the “Why Public Health Matters” campaign continues to receive video submissions from a range […]

de Beaumont Foundation Recertified as Great Place to Work
For the second consecutive year, the de Beaumont Foundation has been certified as a Great Place to Work. The designation […]

Dealing With Harassment in Public Health
Acting in the best interests of our communities can sometimes make public health practitioners unpopular figures; pushback to the decisions […]
